Skull Biomaterials
On this Page
Synthetic Implants Used In Aesthetic Skull Reshaping Surgery
Skull reshaping surgery fundamentally consists of either augmentation, reduction or combinations thereof of various contours of the bone (top, front and back of the head) or muscle. (sides of the head) While reductions involve the removal of bone or muscle, any form of augmentation almost always means adding a biomaterial (synthetic implant) to create the effect. Its is helpful for patients to understand what these biomaterials are, when they are used and what the advantages and disadvantages are of their use.
Bone Cements
The application of bone cements to the surface of the skull is the historic method of alloplastic inlay reconstruction of full-thickness defects and onlay contouring augmentations. There are two fundamental types of bone cements, PMMA (polymethylmethacrylate) and HA. (hydroxyapatite) Both are similar in one aspect, they are powder and liquid mixtures that when put together create a moldable putty that can be intraoperatively shaped and allowed to set. But beyond these visible physical similarities they are otherwise quite different.
PMMA is the oldest cranioplasty material and has been used in the skull since 1940. It is a virtually identical to the bone cements that are used in orthopedic surgery to anchor artificial joints, hence the name. PMMA has excellent tissue compatibility even though it is a form of plastic. (Plexiglass)

When mixed, shaped and cured it forms a very hard structure that is highly resistant to fracture. It is also not adversely affected by a wet environment during the curing process. Because it is a plastic material it does not truly bond to the bone and a scar interface forms between the two. This does not affect, however, its stability. It has the advantage of being able to add antibiotic powders when mixed which allows for a sustained postoperative release. The advantages of a PMMA skull augmentation are its ease of shaping during curing, resistance to being wet during the curing process and its lower cost.
HA is a true bone cement in that it actually bonds to the skull bone without a scar interface, otherwise known as osseous integration. Being usually composed of calcium phosphate derivatives, of which makes up a large percentage of the inorganic composition of human bone, it allows for some bone ingrowth into the material. It was originally developed in the 1990s as a frontal sinus and skull bone defect reconstructive material, it has long been also used as a skull contouring material. Despite these favorable biologic properties it is a far more sensitive working material that requires a dry operative field for application. This usually means a wide open field that only a long scalp incision can create. It is also much more costly being over 10X greater in cost than PMMA material per gram.

Custom Skull Implants
For many skull augmentations, the fabrication of a custom skull implant from the patient’s 3D CT scan is the preferred method which has many advantages. By preoperative designing complete control over the augmentation’s shape, dimensions, contours, and edging is done before surgery. As the main reason for skull augmentation revisions is for undesired shape or visible/palpable edging, a custom skull implant design goes a long way to virtually eliminating the lack of smooth contours or implant-bone interface issues.
While there are a variety of materials by which custom skull implants can be made (silicone, PMMA, PEEK, PEKK, HTR, Porous Polyethylene and Hydroxyapatite), and debates can be had about the biologic merits of each of these materials, only one material permits its placement through a small scalp incision. The elastic deformation property of silicone allows its shape to be temporarily changed to permit its insertion through an incision far smaller than the implant’s diameter.

All other skull implant biomaterials are rigid and non-deformable. Thus their placement is gong to require a much longer scalp incision.

Silicone has one of the best biocompatibility of all implanted materials with an elemental number of 14 sitting right below carbon on the periodic table. While many associated silicone with its use in breast implants, custom skull implants are composed of a solid silicone material which can not degrade, break down or ever need to be replaced due to device failure.
Custom Implants vs Bone Cements
While both bone cements and custom implants can be used for skull augmentation, their aesthetic effects and placement techniques differ significantly. This is best understood by the following comparison table on a 1 to 4 rating scale. (4+ = best, 1+ + worst)

| Property | Bone Cements | Custom Implants |
|---|---|---|
| Biocompatibiilty | +++ | +++ |
| Shape Control | ++ | ++++ |
| Surface Area Coverage | + | ++++ |
| Scalp Incision Length | + | ++++ |
| Aesthetic Revision Risk | ++ | ++++ |
| Infectivity Risk | ++++ | ++++ |
| Ease of Modification/Replacement | + | ++++ |
| Cost | +++ | ++ |
To best summarize these differences bone cements requires much larger scalp incisions for placement than custom implants and cover less skull surface area with far more unpredictability in having a smooth shape and the desired aesthetic effect. As a result, bone cements have a much higher rate of revision and are more difficult to modify or replace. While custom implants cost more than bone cements their larger surface area coverage and controlled preoperative design/shape results in higher aesthetic satisfaction with a much lower revision risk…which justifies their increased cost. Both bone cements and custom implants have a remarkably low infectivity risk which does not seem to differ between them.
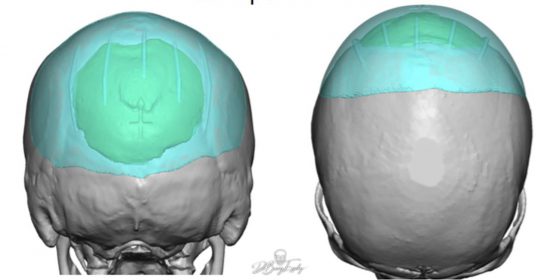
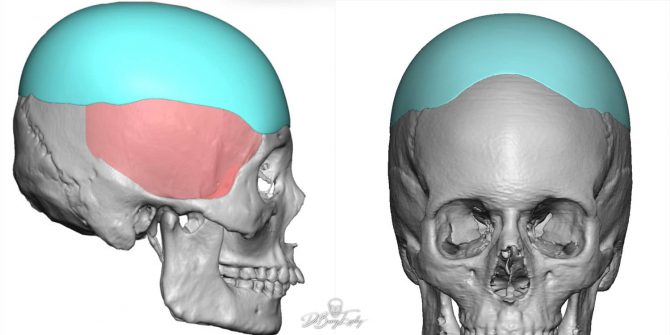
These differences are best illustrated in this case where a custom skull implant (teal color) was used to replace a prior inadequate bone cement augmentation (green color) of the back of the head.
ePTFE
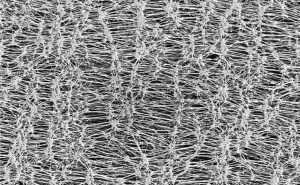
For some small skull defects or for the addition of material to enhance a prior skull augmentation procedure, the use of ePTFE (expanded polytetrafluoroethylene) can be useful. With a long history of use in the face with good compatibility and tissue ingrowth to its microporous surface, its availability in sheets of different thicknesses makes it an adaptable material. It can be easily cut and shaped to be applied directly to bone or onto an implant’s surface or edge.
Screws

Screw fixation is often used for most custom skull implants and in some bone cement cranioplasty procedures. The purpose is to either fix a custom skull implant into an assured position prior to scalp closure or to give the bone cements purchase points for adherence. In either case the screws used are fairly small and they are composed of nearly pure titanium metal. Being element #22 on the periodic table this material offers high strength and is corrosion resistant. It also is a non-ferromagnetic metal which means it does not respond to magnetic forces making it safe for patients to have MRIs and not being detectable in airport scanners.
Locations
Carmel, IN 46032 USA
Contact Us
